We’re going to be closing out National Family Caregivers Month with interviews and information about adult day care programs in Washtenaw County. Recently we spoke with Tina Berry of Huron Valley PACE. A member of the National PACE Association, Huron Valley PACE helps older adults continue to age in place in their home by offering a full continuum of care.
Ahead of the Curve: If you had to give an “elevator speech” about what your organization does, how would you describe it?
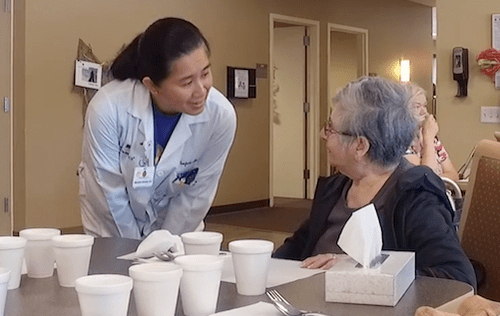
Tina Berry: Huron Valley PACE is a Program of All-Inclusive Care for the Elderly. Our mission is to help older adults continue living in their homes and avoid moving to a nursing home as their care needs increase. We coordinate and provide medical and support services. Our team includes a medical doctor and team of clinicians, nurse and social work case managers, pharmacy, rehab and restorative therapies, home care, nutrition services, recreation and social support, transportation, medical equipment and supplies, and more! Services are provided in your home and in our Day Health Center.
AOTC: Walk me through the step-by-step process. What happens when you get a phone call/referral?
TB: The following happens when we get a referral:
- Our enrollment team will answer your questions about PACE and provide information. If it sounds like a service you are interested in, we will do a screening for eligibility over the phone.
- An Intake Staff Member will visit you at your home to have a more detailed conversation and obtain your written permission to verify medical records and insurance. If you need help applying for long-term care Medicaid (which makes PACE services free), we will begin helping you apply.
- The PACE primary care physician and social work case manager will visit you at your home (or you can come see them at the PACE Day Health Center) to get to know your care needs better, determine eligibility and begin a plan of care.
- If eligible, you sign enrollment paperwork and finalize any insurance applications with the Intake Staff Member.
- Services are effective on the following first of the month.
AOTC: What organizations do you work closely with?
TB: PACE has close partnerships with the University of Michigan, St. Joseph Mercy and IHA for specialist medical care and acute medical needs. Huron Valley Ambulance provides our medical transportation and after-hours emergency call support. HomeTown Pharmacy provides our prescriptions. PACE also contracts with a number of sub-acute rehab facilities, adult foster care and group homes, assisted living and skilled nursing facilities, as well as home care agencies, durable medical equipment and other medical suppliers. A complete provider directory is provided to every new enrollee.
AOTC: What are some things you wish the public knew about your role?
TB: PACE services are entirely free to people with income under $2349/month who meet the MDHHS asset limits. Many people do not have Medicaid insurance prior to calling PACE. We help them get the insurance they need. There is no cost to the intake process.
Huron Valley PACE is a long-term support service. Unlike the in-home services you might receive following a hospital discharge, PACE services are designed to care for you for the rest of your life. Finally, your care team with PACE has incredible flexibility to partner with you in staying independent and preventing health care crises. We want to start providing services as soon as you are eligible!
AOTC: What tips do you have for someone with a loved one that’s going through this issue/needs assistance?
TB: Don’t wait to call us! Call as soon as you notice you need help. Even if you’re not eligible quite yet, we can be your safety net and start providing services as soon as you are.
Common ways people meet the level of care criteria for enrollment include needing hands-on help with activities of daily living (e.g., getting up from a chair or other surface, using the toilet and cleansing or changing incontinence products, eating), short terms memory problems that require another person to help manage your day-to-day life, hallucinations or delusions, dialysis or daily oxygen that impacts daily functioning, and/or an ongoing need for therapy with treatment from physical, occupational or speech therapy in the last week.
AOTC: Is there anything you would like to add?
TB: PACE services look different for each participant in our program. Our plan of care is tailored to the individual needs of each person. Call us to begin getting the support you need to stay at home!
Thank you to Tina for sharing information about this valuable community program!
You can learn more about Huron Valley PACE by calling them at (734) 572-5777 or visiting their website
Visit the Ahead of the Curve Resource Directory for information about other caregiver resources in the community.